The subject of smear testing might not be the most comfortable or glamorous topic, but it’s such an important part of keeping you healthy. My goal is to make sure you feel completely informed and confident about the process, your results, and what might happen next. So, let’s break it all down together.
Who Needs a Smear Test?
In the UK, we recommend cervical screening (or smear tests) for anyone with a cervix between the ages of 25 and 64.
Here’s how often you should have one:
- If you’re 25–49 years old: Every 3 years.
- If you’re 50–64 years old: Every 5 years.
The idea isn’t to look for cancer—it’s actually to catch any early changes in your cervical cells that could potentially develop into something more serious. It’s a preventative measure, not a diagnostic test.
What’s the Smear Test Looking For?
When we do a smear test, we’re looking for two key things:
1. HPV (Human Papillomavirus):
This is a very common virus, and certain high-risk strains can sometimes cause changes in the cells of your cervix.
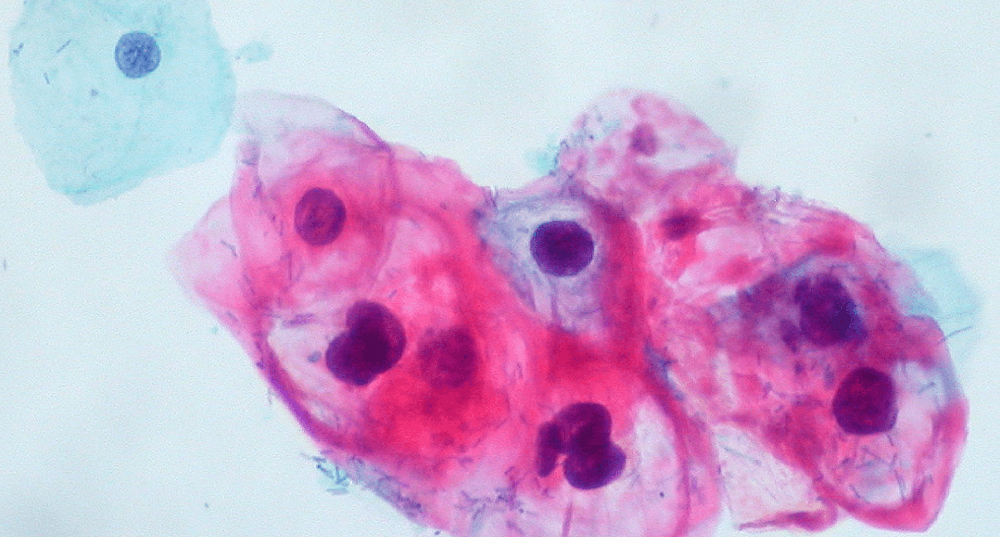
2. Abnormal Cervical Cells:
If we find changes, we use a system called Cervical Intraepithelial Neoplasia (CIN) to describe how mild or severe those changes are:
CIN 1: Mild changes that often go back to normal on their own.
CIN 2: Moderate changes that we might need to treat to prevent progression.
CIN 3: Severe changes that carry the highest risk of developing into cancer if untreated.
How the HPV Vaccine Helps
The Human Papilloma Virus vaccine, has been a real game-changer. In the UK, it’s routinely offered to girls and boys around the age of 12 or 13. The vaccine helps to prevent infection with risk strains of HPV, like HPV 16 and 18, which are responsible for most cervical cancers.
Here’s why the vaccine is so impactful:
- It’s already reducing HPV infections and the number of abnormal smear results we’re seeing.
- It protects against the most dangerous strains of the virus, significantly lowering the risk of cervical cancer.
You might be wondering why we don’t vaccinate or routinely screen women younger than 25. This is because younger women’s immune systems are fantastic at fighting off HPV, especially if they’ve been vaccinated. Most of the time, their bodies clear the virus naturally within a year or two, and any mild changes in their cervical cells (like CIN 1) often go back to normal on their own. This is why we wait until 25 to start screening—it avoids unnecessary treatment.
What Your Smear Test Results Mean:
HPV-Positive, No Abnormal Cells
If you’ve had a smear that has shown high-risk HPV but don’t see any abnormal cell changes, there’s no need to panic. HPV is incredibly common, and for most people, it clears up on its own.
Next Steps: You’ll typically be asked to have a repeat smear test in 12 month’s time. If the HPV has gone, there’s no further action needed, and you would go back to having the routinely scheduled smear tests (according to your age).
HPV-Positive with Abnormal Cells
If both high-risk HPV and abnormal cells are found, we’ll look at how severe those changes are (CIN 1, 2, or 3).
-
CIN 1: Mild changes that often resolve on their own.
-
CIN 2 or 3: More significant changes that usually need treatment to prevent cancer from developing.
Next Steps: This is when patients typically come to see me. At this stage, we need to take a physical look at the cervix, using a procedure called colposcopy.
Inadequate Sample
Sometimes, we don’t get enough cells to give a reliable result. This could happen if the sample was obscured by blood or mucus or if there weren’t enough cells collected.
Next Steps: You’ll need to repeat the test in about 3 months.
CGIN (Cervical Glandular Intraepithelial Neoplasia)
This is a rarer finding that involves the glandular cells in your cervix, which produce mucus. CGIN can also progress to cancer if untreated.
Next Steps: We’ll need to investigate further with a colposcopy and possibly a biopsy.
What Happens During a Colposcopy?
Colposcopy is detailed examination of your cervix using a special magnifying instrument. Here’s what happens:
1. Getting Ready:
You’ll lie down with your legs supported, and we’ll insert a speculum (just like during a smear test) to gently open the vagina so that I can see the cervix.
2. Looking Closely:
I’ll use a colposcope – a bit like a microscope, which stays outside your body, to enlarge the view of your cervix. I’ll also apply a vinegar solution (acetic acid) to highlight any abnormal areas.
3. Staining the Cells:
I may gently paint some iodine solution on to the neck of the womb to stain the healthy cells. This makes abnormal cells easier to spot.
4. Taking a Biopsy (if needed):
If I see anything unusual, I may take a small tissue sample. You might feel a quick pinch, but it’s over in seconds.
5. Treatment (if needed):
Sometimes, we can treat abnormal areas during the same visit. This could involve ‘LLETZ’.
LLETZ stands for ‘large loop excision of the transformation zone’, a procedure to remove an area of the cervix where abnormal cells have been detected. Sometimes, during colposcopy, I will carry out a LLETZ procedure if I see cell changes that I think need treating there and then. LLETZ can also treat areas of abnormal cervical cells after we have the biopsy results.
The neck of the womb is first numbed with a local anaesthetic injection, and the abnormal area is removed using a heated wire in the shape of a small loop. This also seals the tissues, and the entire procedure takes around 15 minutes. Some women choose to have the LLETZ performed under a general anaesthetic.
It’s important to be aware that for 24 hours before the procedure, you should avoid vaginal sex or the use of vaginal creams. It’s nearly always possible to have a colposcopy whilst you have a coil in situ.
Afterwards:
You might have some light bleeding or discharge for a few days, so it’s best to avoid tampons and sex for about a week to let your cervix heal.

FAQ about Smear Tests
1. Does an Abnormal Smear Test Mean Cancer?
No. Most abnormal results are signs of precancerous changes, not cancer itself. The smear test is designed to catch these changes early, so they don’t progress.
2. Why Do I Still Need Smear Tests if I’ve Had the HPV Vaccine?
The vaccine is highly effective, but it doesn’t cover all types of HPV. Regular screening is still the best way to stay on top of your cervical health.
3. Can CIN Go Away on Its Own?
Yes, especially CIN 1. Often, your immune system can clear the virus, and the cells will return to normal without any treatment.
If you’re feeling concerned about an abnormal smear test result, please book an appointment and come and see me.