Endometriosis isn’t just a women’s health issue—it’s a life-altering condition that affects every part of a person’s wellbeing, from their physical health to their emotional resilience and relationships. And yet, despite its enormous impact, it’s still frequently misunderstood, misdiagnosed, and overlooked.
As someone with extensive experience in gynaecology, I’ve met hundreds of endometriosis patients whose journeys have been shaped by pain, frustration, and delayed diagnosis. My mission is simple: to help people living with endometriosis feel seen, heard, and supported—and to offer practical, evidence-based help every step of the way.
I’ll be explaining what endometriosis is, what symptoms to look out for, how it’s diagnosed and treated, and most importantly, how to live well with this chronic condition. Whether you’re newly diagnosed or have been living with endometriosis pain for years, I hope you find reassurance, clarity, and guidance here.
What Is Endometriosis?
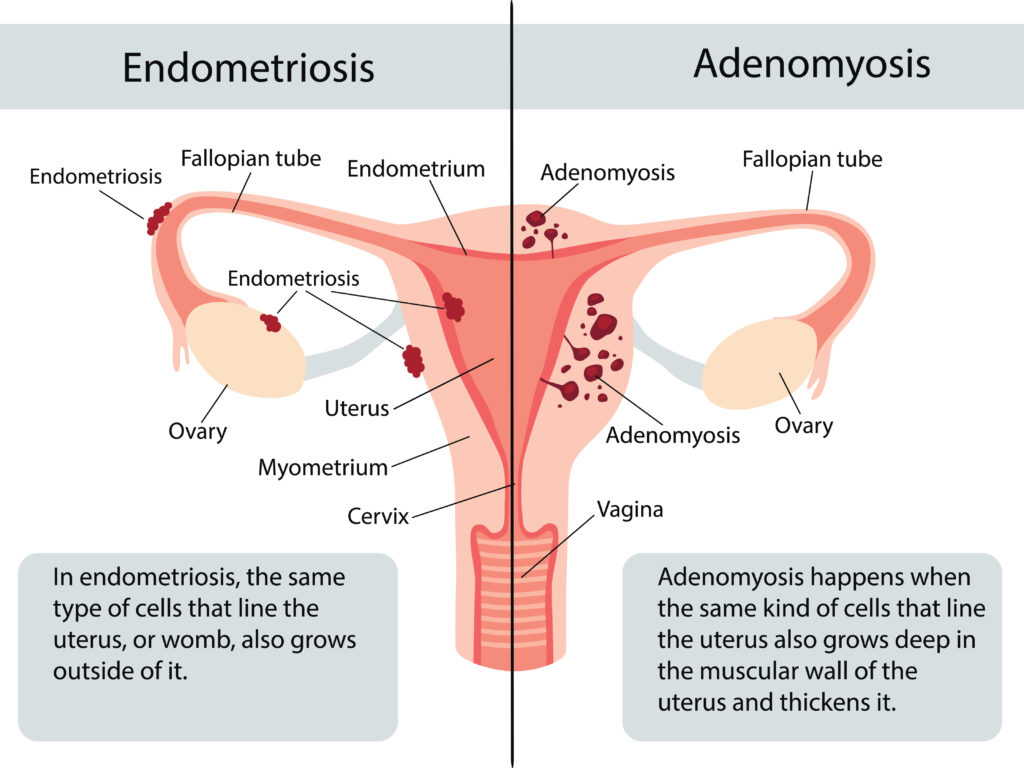
Endometriosis is a condition where tissue similar to the lining of the uterus—called endometrial tissue—starts to grow outside the womb. These growths, known as endometriosis lesions or endometrial implants, can appear on the ovaries, fallopian tubes, bowel, bladder, or in the pelvic cavity, and in some rare cases, even outside of the pelvis.
Each month, this tissue behaves like the lining of the uterus: it builds up, breaks down, and bleeds. But unlike a menstrual period, the blood from this tissue has nowhere to go, leading to inflammation, scarring, and the formation of ovarian cysts, sometimes called ovarian endometriomas.
There are different forms of endometriosis, including:
- Superficial endometriosis: Found on the surface of pelvic organs.
- Deep infiltrating endometriosis (DIE): Where tissue grows into the walls of pelvic organs or the uterosacral ligament.
- Endometriotic lesion clusters that can spread and bind organs together, causing adhesions.
Endometriosis Symptoms
The symptoms of endometriosis vary widely—some people with extensive disease have mild symptoms, while others with minimal disease experience severe pain. The most common signs include:
- Pelvic pain, especially during menstruation
- Chronic pelvic pain that persists throughout the month
- Painful periods (also called dysmenorrhoea)
- Pain during intercourse (dyspareunia)
- Pain during bowel movements or urination, especially during your menstrual cycle
- Heavy periods or heavy menstrual bleeding
- Fatigue, nausea, or bloating
- Difficulty conceiving (infertility)
If these symptoms sound familiar, and particularly if they’ve been happening for years, you might have suspected endometriosis. Unfortunately, many patients are dismissed or misdiagnosed with conditions like pelvic inflammatory disease, irritable bowel syndrome (IBS), or psychological distress before a proper endometriosis diagnosis is made.
What Causes Endometriosis?
The exact cause remains unknown, but several theories exist. One leading explanation is retrograde menstruation, where menstrual blood flows backward into the pelvic organs, carrying endometrial cells that implant and grow. However, this alone doesn’t explain all cases—many people with retrograde menstruation don’t develop the condition.
Other contributing factors may include:
- Genetics (a family history increases risk)
- Immune system dysfunction
- Environmental exposures
- Hormonal influences during reproductive age
It’s also possible that some people are born with endometrial cells misplaced during foetal development, which later respond to hormones.
Endometriosis Diagnosis- Why it’s Often Delayed
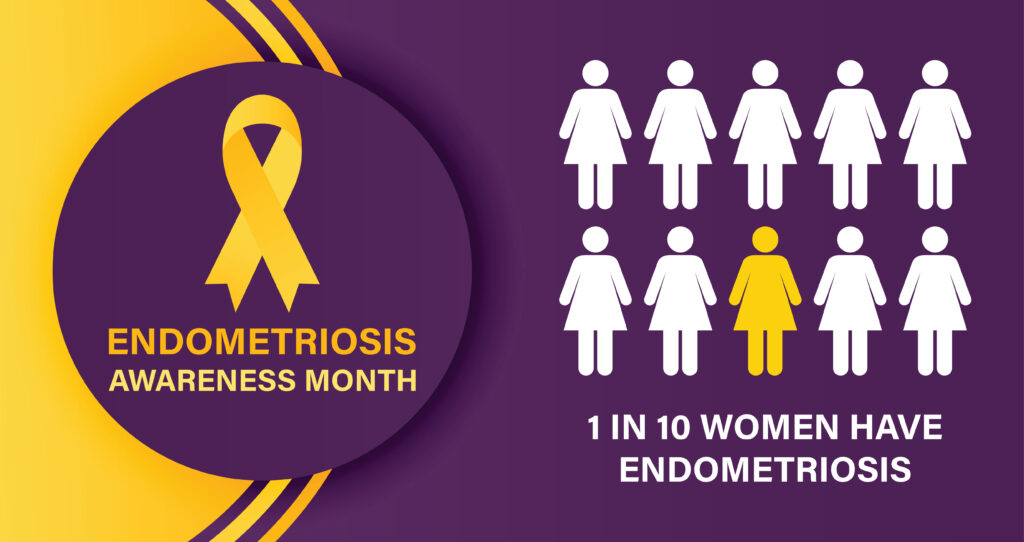
On average, it takes 7 to 10+ years for a diagnosis to be confirmed. This delay is unacceptable, and it’s something clinicians and campaigners like those at Endometriosis UK and the Endometriosis Foundation are working hard to change.
Diagnosis usually involves:
- A detailed medical history
- Pelvic examination
- Imaging (such as ultrasound or MRI)
- Laparoscopy, a keyhole surgery that allows direct visualisation of endometriotic lesions and often removal or biopsy
It’s important to be examined by someone who truly understands endometriosis. Many early cases or superficial lesions can be missed by general scans or inexperienced clinicians.
Endometriosis Treatment Options
There’s no known cure for endometriosis, but there are several effective treatments that can relieve symptoms and slow progression. Your treatment plan should be based on your personal goals, symptoms, and life stage—whether that’s managing pain, preserving fertility, or improving quality of life.
Here are the most common options:
- Hormone Therapy and Hormonal Treatment
Endometriosis is hormone-dependent, particularly influenced by oestrogen. Hormone therapy aims to reduce or suppress the hormonal fluctuations that trigger lesion growth and menstrual bleeding.
Options include:
- Combined oral contraceptives
- Progestins (e.g. the mini pill, Mirena coil)
- GnRH analogues (to induce temporary menopause)
- Aromatase inhibitors
Hormonal treatment for endometriosis can reduce pain and inflammation, but some patients may experience side effects or find it doesn’t fully resolve symptoms.
- Surgery
Surgical treatment, often performed via laparoscopy, allows for excision (cutting out) or ablation (burning away) of endometrial implants, deep endometriosis, adhesions, and ovarian endometriomas.
It’s crucial that surgery is performed by a specialist in endometriosis. Poorly executed surgery may leave tissue behind, cause more scarring, or damage surrounding organs. That’s why I always advocate for referral to a multidisciplinary team with advanced laparoscopic skills.
- Pain Management and Lifestyle
Painkillers such as NSAIDs can help manage period pain, but they don’t address the underlying cause. More holistic approaches include:
- Pelvic physiotherapy
- Diet and nutrition guidance
- Acupuncture
- Mindfulness and cognitive behavioural therapy
- Heat therapy and gentle exercise like yoga or walking

Living with Endometriosis: More Than a Medical Diagnosis
The reality of endometriosis isn’t just physical. It’s emotional, social, and psychological. Patients often describe feeling isolated, misunderstood, or worn down by the relentless nature of endometriosis pain.
At work, many people feel unable to speak openly about their symptoms. In relationships, pain during intimacy or fatigue may create distance. In fertility, the fear of not being able to conceive can be overwhelming.
That’s why supporting people with endometriosis needs to go beyond medication or surgery. It means validating their experiences, listening without judgement, and offering a pathway to long-term support.
Fertility and Endometriosis: What you need to know
One of the most distressing aspects of the condition is its impact on fertility. Around 30-50% of women with endometriosis experience difficulties getting pregnant.
This is often due to:
- Damage or blockage of the fallopian tubes
- Inflammation affecting egg quality or ovulation
- Endometriotic lesions distorting pelvic anatomy
If you’re trying to conceive, early referral to a fertility specialist is essential. Sometimes surgery can help restore pelvic anatomy. In other cases, assisted reproductive techniques like IVF may be recommended.
The good news? Many people with endometriosis do go on to have successful pregnancies—with the right support.
How I Can Help You
I’m deeply committed to improving the lives of people living with endometriosis. In my private practice, I offer a comprehensive service that includes:
- Accurate diagnosis using advanced imaging and laparoscopic assessment
- Tailored treatment plans that include hormonal and surgical options
- Multidisciplinary support, including pelvic physio, nutritionists, and fertility experts
Whether you’re at the beginning of your journey or have been fighting for answers for years, I want you to know this: You are not alone. Endometriosis can feel like a heavy burden, but with the right care, it’s possible to reclaim your health, your energy, and your future.
Final Thoughts
If you’re reading this and recognising your own story in the symptoms described, don’t wait. Too many people suffer in silence or are told that painful periods are “normal.” They’re not. Endometriosis symptoms are real, and they deserve to be taken seriously.